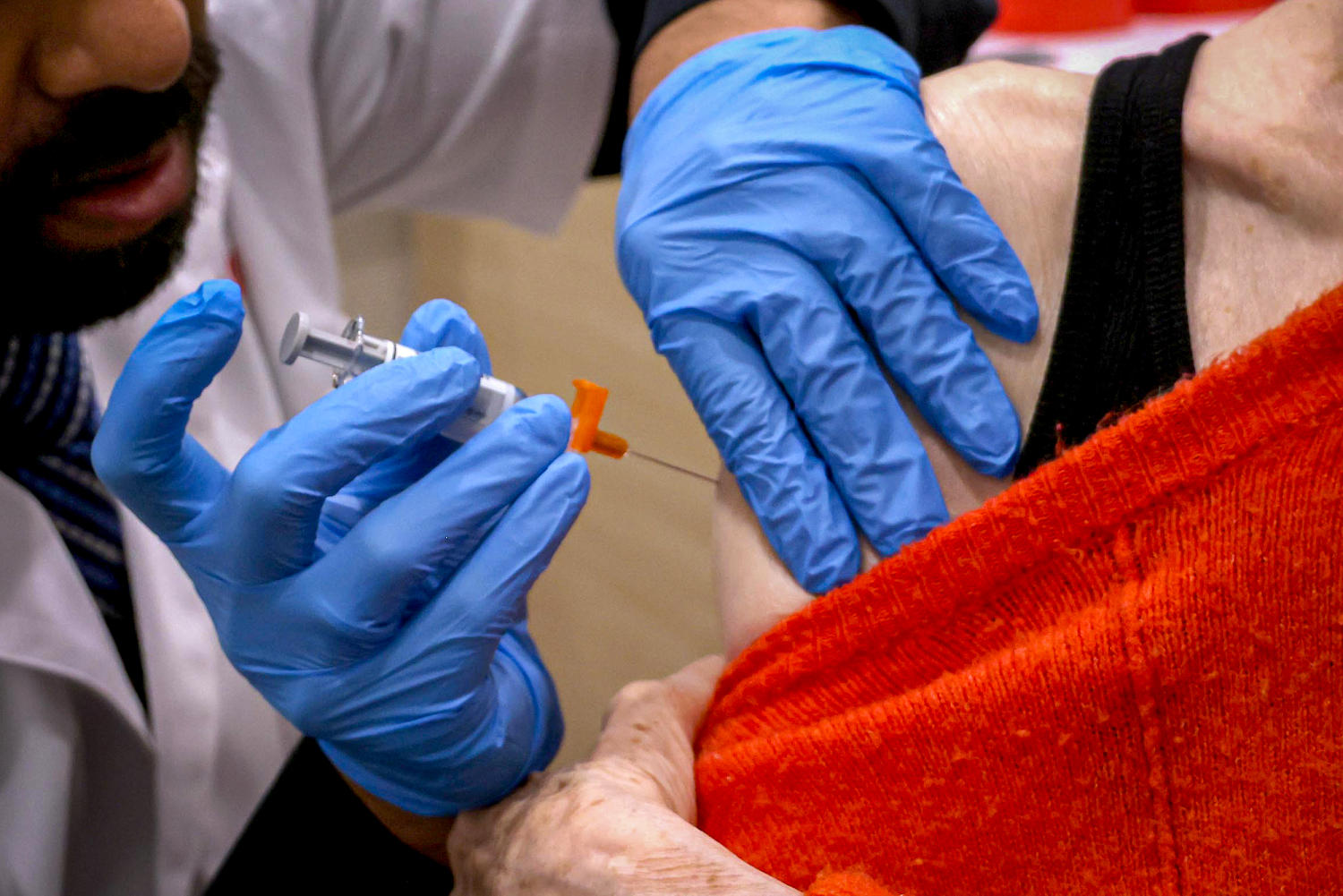
In October, the Centers for Disease Control and Prevention recommended that high-risk adults get a second updated Covid vaccine to bolster their protection against the virus.
The agency now recommends that people ages 65 and up and those with weakened immune systems get a second dose of the 2024-25 vaccine six months after their first dose.
It’s not the first time the agency has advised or allowed for an additional dose for at-risk groups several months after the first. In the spring of 2022, officials authorized a second booster dose after the initial fall rollout. The same pattern followed in the spring of 2023 and the spring of 2024.
No other vaccines are given at such a high frequency, but experts say there’s no reason to believe that the vaccines — and in particular, the mRNA vaccines from Pfizer and Moderna — aren’t effective.
Pfizer’s and Moderna’s vaccines were the first to use mRNA technology to induce immunity to a virus, an approach that proved critical in the early days of the pandemic because mRNA vaccines can be developed much faster than traditional vaccines.
Despite the CDC recommending an additional shot, there’s no evidence that the mRNA vaccines aren’t working as expected, said Akiko Iwasaki, a professor of immunology at the Yale School of Medicine.
Rather, Iwasaki said, there may be something unique to this virus that is preventing people’s bodies from maintaining high levels of immunity.
A recent study from researchers at Emory University found that so-called hybrid immunity — when a person has been both vaccinated and infected with the coronavirus at some point — failed to significantly establish certain long-lasting cells that secrete antibodies. That wasn’t the case for people who had been vaccinated against the flu and tetanus, suggesting, Iwasaki said, that something different is happening with the virus.
“You would think that kind of hybrid immunity is going to be the most rigorous, and yet they did not see increases in these long-lived plasma cell numbers,” she said.
Dr. Ashish Jha, dean of the Brown University School of Public Health and the former White House Covid-19 response coordinator, said there is some uncertainty about the durability of the mRNA vaccines compared to older vaccines technologies.
“Maybe it is a little less durable,” Jha said. “I would say we don’t know.”
The bigger issue, Jha said, is how rapidly the virus mutates, as well as its year-round presence.
“The problem here in my mind is not so much with the vaccine but much more with the virus,” he said, adding that he supports the updated guidance.
“It’s what I’ve actually been recommending to my own parents and it’s what I have said publicly,” he said.
The guidelines come amid concerns that waning vaccine immunity, particularly in older adults, may leave them more vulnerable to severe disease and hospitalization.
“Topping off your vaccine-induced immunity every six to 12 months is not a bad idea,” said E. John Wherry, an immunologist at the University of Pennsylvania. The vaccine bolsters antibody levels, which are the first line of defense against the virus, he added.
“That makes it easier for the rest of your immune system to clean up and prevent that little bit of infection-causing disease,” Wherry said.
A rapidly changing virus
“We look at our flu vaccine strains every year and try to match them up as best we can,” said Dr. Anna Durbin, an infectious disease physician and associate professor at the Johns Hopkins University School of Medicine. “It’s changing even faster with Covid — it’s constantly mutating to get the advantage.”
One reason there aren’t frequent boosters for a virus like measles is because it doesn’t change as rapidly as the coronavirus.
“A measles virus that you encounter today is very similar to a measles virus that you might have encountered five years ago or 10 years ago,” Jha said.
In a perfect world, the Covid vaccines would be able to be updated much faster to match the strains in circulation.
“By the time we pick which strain of Covid we’re going to switch the vaccine to, and by the time that vaccine is ready and rolled out, the virus has already mutated some,” Durkin said. “So the thought really is, can we boost immunity that may not be a perfect match to the strain circulating?”
If that immunity is boosted with another dose of the vaccine, we’ll be able to better protect those high-risk people, she said.
Jha doesn’t expect the twice yearly vaccine to become a universal recommendation for all age groups, as the immune system of a 30-year-old is far more robust than that of an 80-year-old.
“Unless the virus gets more virulent,” he said. “Which I don’t really think is going to happen.”
